
Qian Hu1, 2, 3, Shi-Hua Zheng1, 2, 3, Wei Liu1, 2, 3
1The First College of Clinical Medical Science, China Three Gorges University, Yichang, China.
2 Institute of Digestive Disease, China Three Gorges University, Yichang, China.
3 Department of Gastroenterology, Yichang Central People’s Hospital, Yichang, China.
*Corresponding author: Wei Liu, Ph.D., Institute of Digestive Disease, China Three Gorges University, 8 Daxue Road, Yichang 443000, China.
Received Date: November 25, 2023
Accepted Date: December 08, 2023
Published Date: December 29, 2023
Citation: Hu Q, Shi-H Zheng, Liu w. (2023) “Abdominal Tuberculosis.” Case Reports International Journal, 1(1); DOI: http;//doi.org/10.2023/12.1003.
Copyright: © 2023 Wei Liu. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
A 67-year-old woman presented with abdominal pain for the last month. She denied a history of cough, fever, nausea, vomiting, diarrhea, and weight loss. She had no similar complaints in the past. Physical examination revealed mild abdominal tenderness.
Introduction
A 67-year-old woman presented with abdominal pain for the last month. She denied a history of cough, fever, nausea, vomiting, diarrhea, and weight loss. She had no similar complaints in the past. Physical examination revealed mild abdominal tenderness. There were no signs of hepatomegaly and splenomegaly. Laboratory tests showed mild anemia and elevated sedimentation rate. The AFP, CA19-9, and CEA were normal. Autoimmunologic test and immunoglobulin (Ig)G4 were normal. The T-SPOT.TB test was positive. Normal lungs were shown by computed tomography (CT) of the chest. Abdominal contrast-enhanced CT scan showed a 5.7 × 4.5cm ill-defined oval mass of soft-tissue density above the neck of the pancreas, and hilar lymph nodes enlargement and necrosis (Figure 1A).
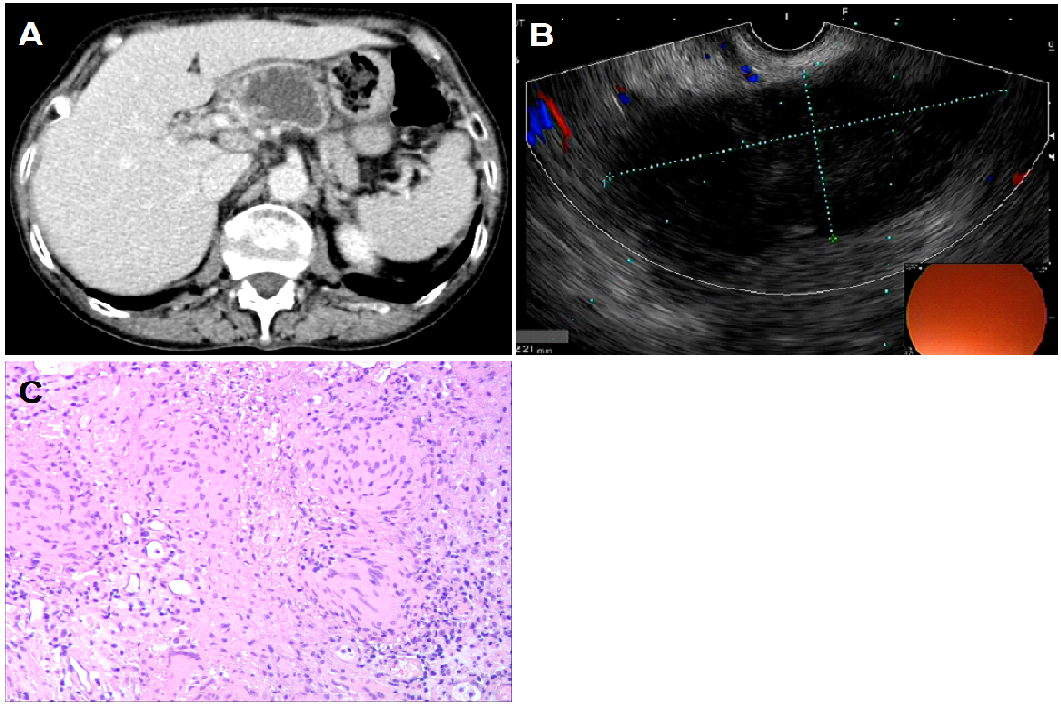
Figure 1. A. Abdominal contrast-enhanced CT scan showed a 5.7 × 4.5cm ill-defined oval mass of soft-tissue density above the neck of the pancreas, and hilar lymph nodes enlargement and necrosis. B. The lesion was cystic component with heterogeneous hypoechoic cavities by endoscopic ultrasonography. C. The histopathological examinations confirmed necrosis and granulomatous lymphadenitis.
The lesion was cystic component with heterogeneous hypoechoic cavities by endoscopic ultrasonography (EUS). (Figure 1B). Doppler confirmed no abundant blood flow. Fine-needle aspiration (FNA) was done on both the lesion and the adjacent enlarged lymph nodes. The histopathological examinations confirmed necrosis and granulomatous lymphadenitis (Figure 1C). No malignant cell was found. Polymerase chain reaction testing for M tuberculosis was positive. Colonoscopy and upper gastrointestinal endoscopy revealed no signs of digestive tract tuberculosis. Finally, we reached a diagnosis of abdominal tuberculosis. The lesion was isolated and localized to the pancreaticohepatic area considering normal chest CT, colonoscopy, and upper gastrointestinal endoscopy. She took a standard course of 4 anti-TB drugs: isoniazid 0.3 g, rifampicin 0.45 g, pyrazinamide 1 g, and ethambutol 0.75 g QD. One month after antituberculous medication, her symptom of abdominal pain significantly improved. In conclusion, peripancreatic tuberculosis may mimic malignant pancreatic tumors in signs, symptoms, and radiographic examinations, which is a rare cause of abdominal pain.1-3 Endoscopic and molecular techniques may increase the success rate of diagnosis and avoid risky surgical procedures.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this “GI Image”. Board institutional approval was not required.
Author’s contributions
Collection of data and writing: Qian Hu.
Manuscript preparation: Shi-Hua Zheng.
Final approval of the manuscript: Wei Liu.